|
|
|
Repeat Surgical Procedures When your Carrier doesn't like modifier 76 Last Updated: 02/24/2018 |
|
When multiple surgical procedures are being billed (e.g., four 11402 excisions, 9 AKs, multiple Mohs removals, multiple additional stages of Mohs, etc.), a number of different questions come into play on how to bill multiple units. 1. Is the code billable in units? 2. Is there a limit under the Medicare Unlikely Edit (MUE) rules? 3. What modifiers are required for additional surgical procedures after the first after the first procedure is billed? When using DermCoder, you can tell a lot of information on the main CPT screen that will help answer many of these questions… Let’s look at at CPT code 11402 as an example… Here we have entered 11402 into the “Code Jump” box in DermCoder to pull up 11402. On the bottom right, you will find two critical pieces of information, MUE (limits) and whether or not the code should be billed in units. 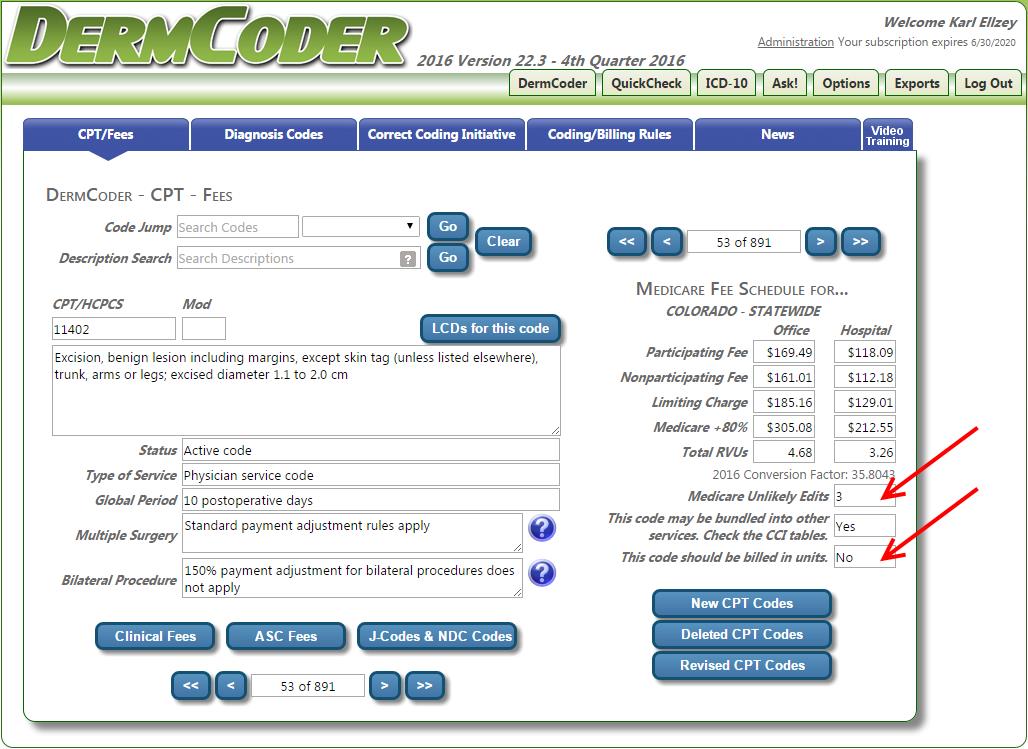 So let’s say you perform four 11402s on a patient with a number of lipomas that were irrated and met the criteria for medical necessity. How would you bill these on a claim? Well, first we know that you would not bill this code in units, because DermCoder guides you and has ‘No’ populated on the main CPT screen under the “Billable in units” field. We also know that our limit is a total of three on a claim before any red flags or automatic denials are created with the carrier. Incorrect way to bill. 11402 x 4 units For a repeat procedure, most carriers accept modifier 76 on the subsequent procedures after the first (for laboratory procedures and test, use modifier 91 for repeat procedures) Correct way to bill… 11402 11402 -76 11402 -76 11402 -76 However, we have exceeded the total number of MUEs (Medicare Unlikely Edits) for this code; so what do you do? Box 19 of the CMS-1500 claim form is known as the claim narrative field. In this field, you should enter a note with the total number of procedures performed on that date. Example: Total of 4 CPT 11402 procedures were performed on 09/07/2016. (If you file electronically, include this information in the Loop 2300/2400 segment of your electronic claims.) Use of the “narrative” field should also help avoid duplicate line item denials. You most likely will have to submit this claim with notes and a cover letter explaining that the total number of procedures exceeded the MUEs, but that the patient met conditions for medical necessity and that the provider deemed it necessary to perform the total number of excisions on that date of service. Be sure to highlight in the medical notes, all of the medical necessity criteria that were met (i.e., irritated, inflamed, etc.) Warning! Not all carriers recognize modifier 76! I know of two Medicare carriers that don’t recognize modifier 76 for surgical procedures. Wisconson Physician Service (WPS) and Novitas. Here are their policies… http://wpsmedicare.com/j5macpartb/resources/modifiers/modifier-76.shtml WPS states… “Inappropriate Usage • Appending to a surgical procedure code” http://www.novitas-solutions.com/webcenter/portal/MedicareJH/pagebyid?_afrLoop=1031902925727321&_adf.ctrl-state=4kidwee4r_118&contentId=00092327#! Novitas states… “Inappropriate Uses: -Adding to a surgical procedure code; -Staged procedures (modifier 58), -Unplanned return to operating room (modifier 78) -Unrelated procedure or service (modifier 79).” So what do you do for repeat surgical procedures when you can’t use modifier 76 and you can’t bill in units? WPS published a Frequently Asked Question (FAQ) in April 2014 http://wpsmedicare.com/j5macpartb/faq/departmental/top-written-faqs-feb-mar-april-2014.shtml Question: We repeated several minor surgical procedures on our patient on the same day. We appended the 76 modifier to alert Medicare that they were repeat procedures and not duplicates, but Medicare rejected the lines containing the 76 modifier indicating the modifier was invalid. How should we bill repeat surgical procedures? Answer: WPS GHA does not recognize modifier 76 for surgery (type of service 2) codes. When multiple units of a surgical procedure are performed, providers should first determine if the code could be quantity-billed. If so, the claim should be submitted with multiple units per line. If the code cannot be quantity-billed, each unit should be submitted on a separate claim line. Indicate in the narrative field the total number of units performed on the date of service in question. For more information, see our article titled, "Proper Billing of the Same Surgical Procedure Code Multiple Times on the Same Day," which you can find by selecting the Resources tab in the upper navigation, then "Modifiers." You can determine whether a code can be quantity billed by reviewing our article, "Systems Quantity Billing for WPS GHA." To locate this article, select the Claims tab in the upper navigation, then "Claims Submission." The article is located in the Claim Reference Articles" section. For WPS you simply bill all four procedures on separate lines (with no modifier) and you include additional information in the narrative field (Box 19) with the total number of procedures performed on that date of service. (If you file electronically, include this information in the Loop 2300/2400 segment of your electronic claims.) Novitas hasn’t provided any additional clarification, except for this tidbit. http://www.novitas-solutions.com/webcenter/portal/MedicareJH/page/pagebyid?contentId=00002655&_afrLoop=1281374890767882#!%40%40%3F_afrLoop%3D1281374890767882%26contentId%3D00002655%26_adf.ctrl-state%3D9ybsrc8o_84 “Report clarifying information pertaining to repeat or duplicate services using block 19 of the CMS-1500 (02-12) claim form or in the Extra Narrative Data segment (Loop 2300/2400) of the ANSI ASC X12 837 Versions of an electronic claim. Utilize this field to report the time of each subsequent or repeat service or the number of times this service needed to be performed.” For Novitas, we believe you handle this the same way… bill each on a separate line, without modifier 76, include a claim narrative in box 19 explaining the total number of procedures perfomed on that date of service. Why not use modifier 59? Some carriers may accept modifier 59 in place of modifier 76, but this is not the norm. Modifier 59 is normally reserved for bundled pairs of codes that appear in the Correct Coding Initiative. Modifier 59 is applied when a distinct surgical service is performed (separate site, lesion, injury, encounter) and is appropriately billable under the circumstances. Note, however, that a CPT code is never bundled/paired with itself within the CCI edits. In other words there is no CCI edit with 11402 in both columns I and II. WPS went so far as to state the following on their Modifier 59 fact sheet… http://wpsmedicare.com/j5macpartb/resources/modifiers/modifier-59.shtml “Inappropriate Usage -Code combination not appearing in the NCCI edits” Noridian Medicare also has policies in place that modifier 59 is not appropriate on code pairs not appearing in the Correct Coding Initiative. Never used: – Code combination not in NCCI – On two of the same codes https://med.noridianmedicare.com/documents/10542/2... Other scenarios… Other CPT codes are more straight forward. Pathology code 88305, for example, is billed in units. You simply bill 88305 on one line times the total number of units. No narrative is needed in box 19 (unless you exceed the MUE limits for that code). 88305 has an MUE of 16. AKs have add-on codes… the first code is billed once (i.e., CPT code 17000) and additional codes are billed in units (i.e., 17003 x 11 units). DermCoder even warns you if you do this wrong… Try entering 88305 three separate times in DermCoder… DermCoder warns you… 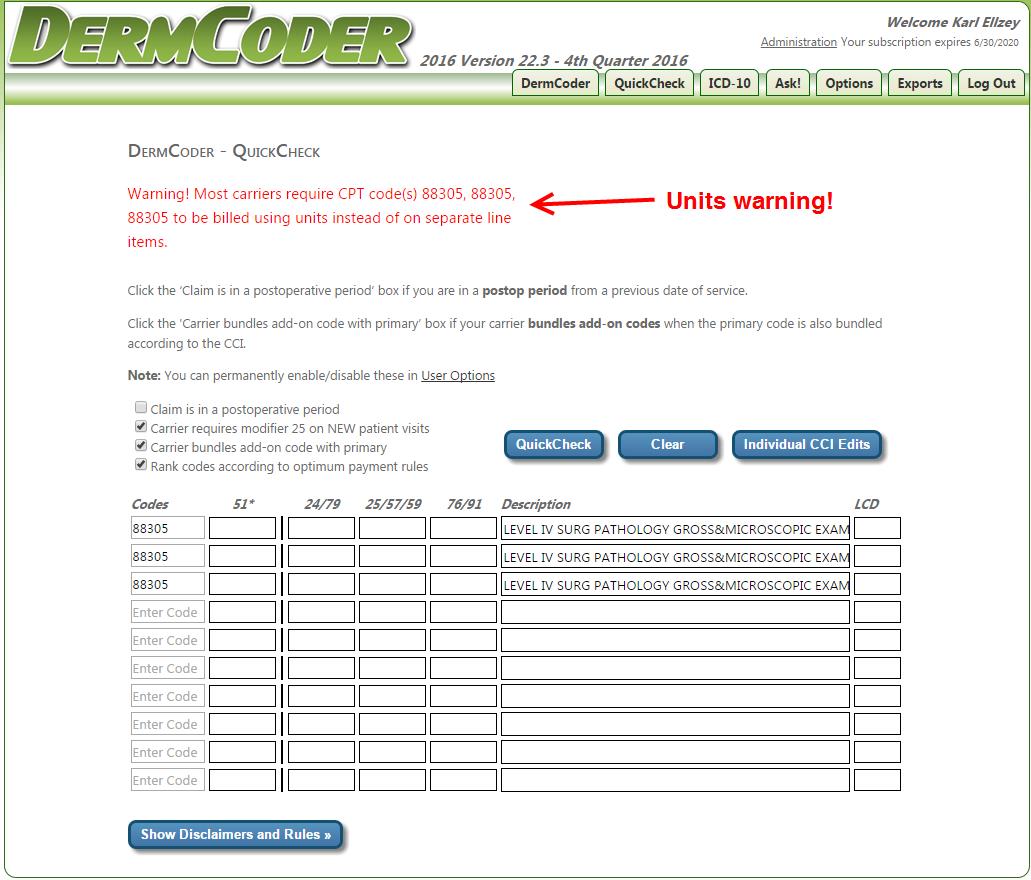 Final words… Most of the time, you can use modifier 76 for repeat surgical procedures (when it can’t be billed in units), unless you have one of the oddball carriers. If modifier 76 isn’t acceptable on repeat surgical procedures, try billing without and use Box 19 (Narrative field) to explain the total number of units performed on that date of service. If necessary, send in the claim with notes and a cover letter. This should hopefuly avoid a duplicate line item denial. Lastly, see if they will accept modifier 59 instead, although that’s not really the correct use of this modifier. Finally, if you are aware of other carriers that won’t accept modifier 76 on repeat surgical procedures, PLEASE send us a note to[email protected] and we’ll update this article. |